Despite the nation’s high rates of coronavirus infections, transitions, and deaths, many U.S. schools reopened for the fall semester.
Some school districts have chosen to adhere to stricter guidelines through remote learning, while others are implementing in-person teaching with specific safety protocols, and others a hybrid of virtual and in-person.
Whatever type of learning, the bottom line is that COVID-19 has not gone away.
Outbreaks are happening, and teaching in school only adds to the risk of spreading coronavirus infection, according to Margie Kochsmier, an infection preventionist with FHN Healthcare System in Freeport, Ill.
“Anyone—including children—can get COVID-19. Generally, children tend to have more mild symptoms, but it’s important to remember that anyone infected with COVID-19 can spread the virus, even if he or she doesn’t show any symptoms at all,” Kochsmier told The Journal-Standard. “The best way we know to avoid the spread of COVID-19 hasn’t changed. Families have to keep their focus on masking, social distancing, handwashing, and keeping surfaces as clean as possible.”
Schools Across U.S. Struggle to Reopen
Despite initial suggestions from the CDC to continue remote learning for the 2020-2021 school year, government officials—including those in the White House—pushed for the opposite.
“I’m shocked that anyone would be shocked to find COVID cases in schools,” said Whitney Robinson, an associate professor of epidemiology at the University of North Carolina’s school of public health, told Education Week. “The only thing that would be shocking is if they didn’t have a plan for it.”
Still, many education experts say that in-person schooling is vital for childhood development.
The American Academy of Pediatrics (AAP), for example, “strongly advocates” that all policy considerations for the coming school year should start with the goal of having students physically present in school.
“Schools play a really central role in children’s lives, and it’s just not possible to deliver all of the services and benefits of schools when you are in a remote learning situation,” Danielle Dooley, a pediatrician and AAP spokesperson, told the Scientific American. “Being around your peers, being around a community of supportive adults—that’s really critical for a child’s development.
“They need that contact with their peers in order to grow.”
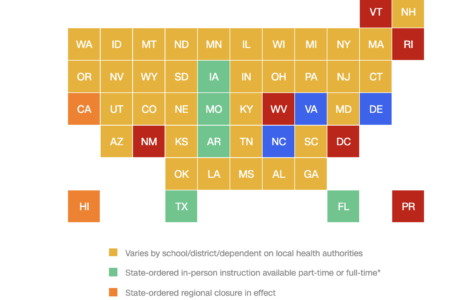
In response to this information, state governments in Iowa, Missouri, Arkansas, Florida, and Texas have ordered schools to reopen. Most other states have chosen to let local school district officials decide which teaching method to implement, according to CNN.
A sad outgrowth of efforts to keep in-person schooling going is that some education officials are requesting that their staff stay quiet about outbreaks.
“Staff who test positive are not to notify any other staff members, parents of their students or any other person/entity that they may have exposed them,” Jon Miller, the Camden County, Georgia’s district deputy superintendent, wrote in a recent confidential email obtained by the New York Times.
In that state, thousands have been forced to quarantine due to possible contact with someone infected with the coronavirus.
Moreover, U.S. universities and colleges are experiencing outbreaks among their student population — many of whom are not adhering to school safety guidelines, according to CNN.
One such campus, Providence College, recently placed 17 students on “interim suspension”—barring them from attending any classes pending a student hearing—for not following the rules.
“I am deeply disappointed by the selfish behavior of these students who defiantly chose to ignore our COVID-19 Code of Conduct,” Fr. Kenneth R. Sicard, Providence’s president, said in a statement. “While I find no joy in having to endorse such strong sanctions, I know they are necessary if we are going to have a successful fall semester.”
Latino children and young adults, who represent 43.8% of COVID-19 deaths in the U.S., face particular risks.
The Path Forward
Mainly, experts say that while teachers, district leaders, or even parents have little control over how their schools decide to move forward during this pandemic, it is vital that every school handles their COVID-19 response uniquely and with flexibility.
“We have to be prepared and flexible for an ever-changing school year,” Danielle Dooley, a pediatrician and spokesperson for the AAP, told the Scientific American. “Protocols and procedures put in place at the beginning of the school year may need to change as the level of disease may increase in a community.”
The AAP has several suggestions for school re-entry policies:
- Be flexible and agile in responding to new information.
- Take a multi-pronged approach to protect students, teachers, and staff.
- Develop strategies that can be revised and adapted depending on the level of viral transmission and test positivity rate throughout the community and in the schools, recognizing the differences between school districts, including urban, suburban, and rural districts.
- Communicate and coordinate with state and/or local public health authorities, school nurses, local pediatric practitioners, and other medical experts.
- Make school re-entry policies practical, feasible, and appropriate for child and adolescent’s developmental stage and address teacher and staff safety.
- Account for the diversity of youth should be made, especially for vulnerable populations, including those who are medically fragile or complex, live in poverty, have developmental challenges, or have disabilities, with the goal of safe return to school.
- Partner with pediatricians, families, and schools to collaboratively identify and develop accommodations when needed for any child or adolescent with unique medical needs.
- Guide school policies by supporting the overall health and well-being of all children, adolescents, their families, and their communities, and create safe working environments for educators and school staff.
- Communicate policies in languages other than English, based on the languages spoken in the community, to avoid marginalization.
AAP also recommends federal, state, and local funding for schools to reopen safely with adequate measures, as well as support for remote learning.
“Funding to support virtual learning and provide needed resources must be available for communities, schools, and children facing limitations implementing these learning modalities in their home … or in the event of school re-closure because of a resurgence of SARS-CoV-2 in the community or a school outbreak,” according to AAP.
Latino parents should inform their school of grave concerns — such as fear of spread among elderly relatives at home, a lack of access to internet services for remote learning, etc.
One way to keep ahead of the information curve is by using The National Education Association’s public school infection tracker, developed by Alisha Morris, a theater teacher in Kansas. This information can give parents the right data to bring to school district leaders if they are concerned with the rising rates of COVID-19 in schools. 
“As our kids become increasingly mobile, they will become part of a large national experiment, and there is little doubt the infection rates will increase,” Dr. Sanjay Gupta, CNN’s Chief Medical Correspondent, writes in a recent op-ed. “Just over the past four weeks, the number of children infected in the United States has increased by 90% to more than 380,000 cases, according to that same analysis by AAP and CHA. While some of that increase may be due to increased testing, younger kids starting to emerge from their homes for the first time also play a role. And, for much of the country, schools haven’t even yet reopened.”
What Can You Do?
If schools are to reopen safely, our communities must also be safe, too.
That’s why Salud America! at UT Health San Antonio launched the “Juntos, We Can Stop COVID-19“ digital communication campaign to help Latino families and workers take action to slow the spread of coronavirus.
The #JuntosStopCovid campaign features culturally relevant fact sheets, infographics, and video role model stories to encourage Latinos to change their public health behaviors.
Share the campaign with your friends, family, and colleagues!
The post Back to School: COVID-19 and Education appeared first on Salud America.
Recommend0 recommendationsPublished in Fit Fiesta Force, Fuerza por la Salud
