Interoperable Patient Records: Its about time
Dr. Rob’s Perspective: Patients—Finally in the Driver’s Seat on Their Health Data
Its my data and its mine if I want it!
By Dr. Rob
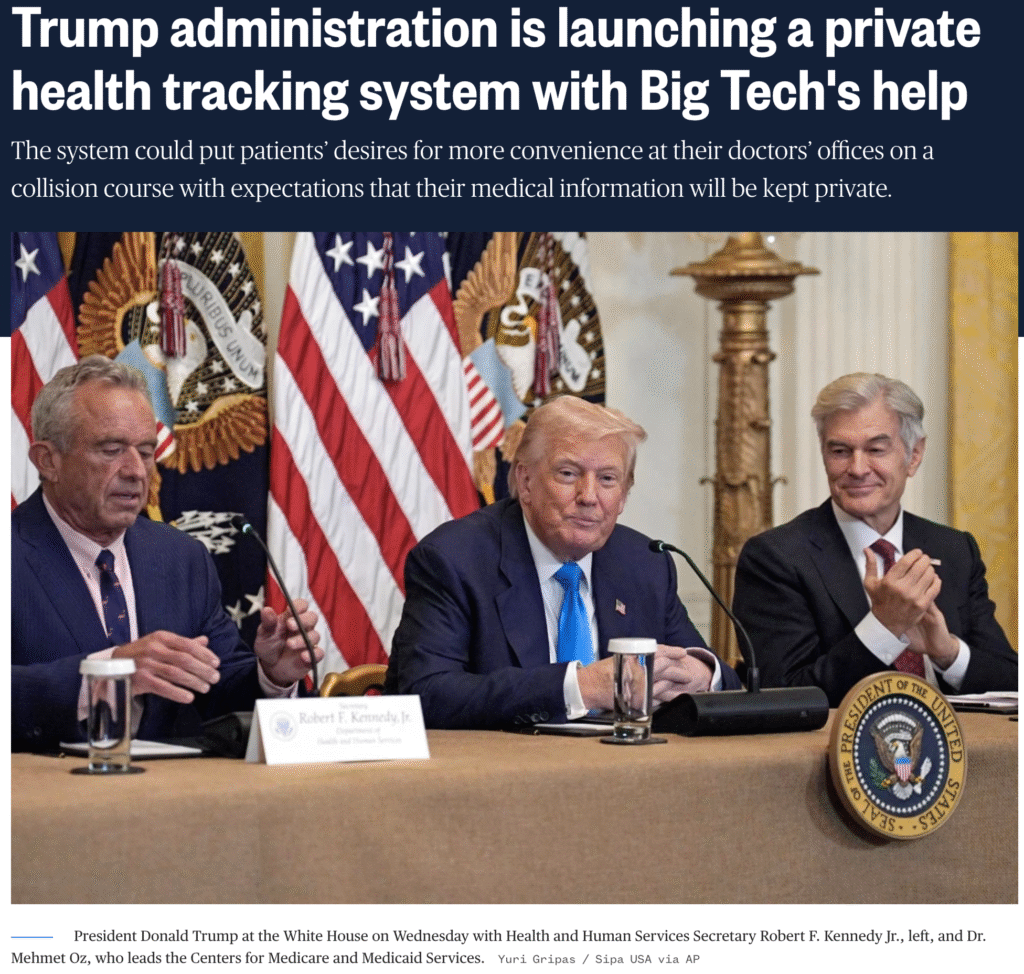
Image is a screenshot from this link: https://www.nbcnews.com/health/health-news/trump-administration-launching-new-private-health-tracking-system-big-rcna222178
This week marks a pivotal moment in U.S. health policy: the Trump Administration unveiled a sweeping initiative compelling EHR vendors and health systems to give patients complete access to and control over their medical records—through any app or platform of their choosing, under an opt‑in model managed by CMS Axios+12Politico+12OncLive+12The Times of India.
Having built my own personal health record (PHR) two decades ago, I’ve witnessed firsthand both the promise and the limitations of early systems. Back then, putting the patient in control was nearly a novelty—not yet practical given limited standards, low interoperability, and weak data portability. Now, with modern APIs based on HL7 FHIR and legal mandates against information blocking, the technology has finally caught up with the vision WikipediaThe National Law ReviewFierce Healthcare.
Why I Support This Initiative
- True ownership of health data: Once exported to a patient‑chosen app or PHR, data is no longer siloed—it belongs to the patient. That means greater agency, consolidation of records, and improved coordination across providers OncLive+4MedicalEconomics+4CMS+4.
- Avoiding duplication and waste: Interoperable access curbs information blocking and makes switching systems—or seeing new doctors—easier and safer, reducing redundant tests and medical errors KFF Health News+6Fierce Healthcare+6The National Law Review+6.
- Enabling innovation in patient tools: Open ecosystems encourage third parties to develop personalized health management apps—especially for chronic conditions like diabetes or obesity, which are among the early focus areas CMS+15TIME+15Politico+15.
Remaining Concerns and Considerations
- Privacy gaps outside HIPAA: Most tech companies (including major names like Amazon, Google, Apple, OpenAI) are not covered entities under HIPAA. Unless there are strong, enforceable privacy agreements, patients risk exposure of sensitive data beyond intended uses—possibly even to advertisers or government agencies in unexpected ways TIME.
- Regulatory clarity needed: Details around consent, secondary data use policies, data retention, and data governance are still emerging. The devil will be in how these rules are enforced—and penalties for misuse.
- Digital equity and usability: Two decades ago, building my own PHR was labor-intensive and discouraged by low digital access and poor interfaces. Even today, health literacy and technology access vary widely—underserved populations must not be left behind.
What I Want to See Next
- Clear legal guardrails on data handling by third parties—including transparency, auditability, revocation options, and strict limits on secondary use.
- Interoperability enforcement with consequences for vendors and providers who resist or delay data portability.
- Usable tools with genuine patient engagement—not just portals with download buttons, but intuitive apps that present data meaningfully and support patients in decision‑making.
- Attention to health equity, ensuring vulnerable populations have device access support, plain‑language consent, and help navigating opt‑in decisions.
Health Literacy is critical
To make the best use of this data and records, a person need to be as health literate as possible use it to advance their health and decisions, and not be scared or confused by what they see. That is why we have been building the Force for Health Network for the last decade. Join for free and start to get health literate and make healthier decisions and ask more informed questions of your providers and policy makers.
In summary, as someone who launched a PHR two decades ago, I’m encouraged to see that the long‑deferred patient‑centered vision is finally being realized. This initiative could transform care—and put patients in true command of their health data—for the first time. But its success will depend entirely on how privacy, usability, and equitable access are implemented in the coming months.
# EHR, #interoperable records, #FHIR, #personal health records, #ForceforHealth, #personal responsibility